How Can An Urologist Help You? with Steven Thoma, MD
Mason City Clinic board certified urologist Steven Thoma, MD, describes the many urologic treatment options for men and women at the Mason City Clinic.
View Transcript
Carol Gifford:
Welcome to Mason City Docs on Call, a podcast series with North Iowa specialists who educate us about how to stay healthy. I’m your host, Carol Gifford. Urology is the medical specialty that focuses on diseases of the male and female urinary system and the male reproductive organs. A urologist treats problems of the kidneys, adrenal glands, urinary, bladder, and male reproductive organs. Because the urinary and reproductive tracts are anatomically linked, problems with one tract often affect the other. Here with us today is board certified urologist Steven Thoma, who will help us understand the key ways the Mason City Clinic Urology Department can be a one-stop shop for men and women in North Iowa. So welcome to the program, Dr. Thoma.
Dr. Steven Thoma:
Thank you.
Carol Gifford:
So first of all, just tell us a little bit about yourself. How did you decide to choose medicine as a career and then subspecialty of urology?
Dr. Steven Thoma:
Sure. So again, yes, my name is Steven Thoma, I am a urologist here at the Mason City Clinic. I’ve been here for just about seven years now, I’m originally from Louisiana. But my wife, who is an ear, nose, and throat doctor, she and I met down in Louisiana, and she’s originally from Ames, so that’s how we ended up back up here a little bit closer to home for her. So yeah, we love it up here, and we really enjoy the clinic here, and being able to serve the patients of North Iowa here. As far as how I got interested into urology, just getting interested in medicine in general, always kind of been that way. My dad is a doctor, he was in emergency medicine, and growing up I would go up to the ER to hang out with him when he was doing shifts, and kind of watch what he did.
And then I always remember growing up seeing his patients, people would just approach us out in public when he wasn’t at work, and just come up. And people that he didn’t even really remember, they remembered him because of the things that he had done to help. And they would come up and thank him, and tell me how great he is, and lucky I was to have him as a dad, which I agree. But just seeing the way that he was able to touch people’s lives, it just was a very special thing. And I just realized that having that opportunity to serve people, to help them with some of these issues that at times can be either very impactful of quality of life or even a threat to their life at times, it means a lot to me to be able to help people in that way.
So eventually once I got into medical school, didn’t really know exactly what field I wanted to be in, but as you do your rotations and you learn things, you kind of learn what fields don’t interest you, and then kind of what fields do. And so urology has been great. I really enjoy the technology that we get to use, there’s robotics, there’s lasers that we get to use. There are some big surgeries, but there’s also quicker things where you can help people in a big way without having to do too much, without having to be too invasive. But then there’s also the medical aspect where there’s things that we can handle non-surgically, and I really enjoy meeting with patients in clinic to be able to help them with that. So it’s a very good mix of medicine and surgery, a lot of ways to help people significantly. And as far as surgical fields go, it’s just a good lifestyle, thankfully not a whole lot of emergencies. So as far as quality of life goes, it’s definitely up there for surgical specialties.
Carol Gifford:
It fits you. Yeah, that’s great. So tell me about the urology department here at the Mason City Clinic. Just tell me how many physicians are in the department, and then what are the medical conditions that you treat?
Dr. Steven Thoma:
Sure. So up until recently there were four urologists. We just had our fifth join us, Dr. Elizabeth Takacs, so there are five now. And we treat the full spectrum of urology. So I guess the more common things that we tend to see would be kidney stones, we see a lot of male voiding dysfunction, so enlarged prostate, difficulties urinating. From the female end of things we see incontinence, urinary tract infections, and then of course we see urologic cancer. So that’s things like kidney cancer, bladder cancer, prostate cancer, testicular cancer, those are going to be things that we treat the most. So full spectrum of urologic care here.
Carol Gifford:
So let’s talk about prostate cancer, because you hear a lot about it. My understanding, it might not be true, it seems like it’s preventable. There’s some test to test for prostate cancer, and if you catch it early, you can cure it, right?
Dr. Steven Thoma:
Sure, yeah. So you use the term preventable. I like to tell guys that there’s no way that we’re going to be able to prevent you from developing prostate cancer, but obviously very treatable, extremely curable if you find it early. And that is our goal with screening and early detection, because absolutely, extremely treatable, highly successful to be cured if found early. And so the mainstay of prostate cancer screening would be the PSA blood tests. PSA stands for prostate specific antigen, it is a normal protein that is made by normal prostatic tissue, but we do know that it tends to go higher, the levels do, in men with prostate cancer. So we use that as a tester, a surrogate, to identify those guys that we should be suspicious might have prostate cancer.
Carol Gifford:
And then if they do have prostate cancer, what are some of the treatments or surgeries for that cancer?
Dr. Steven Thoma:
Sure. So first I’ll step back just a second and touch on something that often draws a lot of anxiety for men when they hear their PSA is high. I always have to explain to guys that just because your PSA is high absolutely does not mean that you have prostate cancer, there are other things that can make that PSA go higher. Things like if you have very large prostate, if you have infection or inflammation of the prostate, if you have significant difficulties with your urination, like you don’t empty your bladder well. And so I always just have to kind of help reassure them that this is not something that is the end of the world, we just need to sort through that. So if you, heaven forbid, ever are found to have prostate cancer, it’s extremely treatable, especially if we find it early. Even when we don’t find it early, it’s still extremely treatable, controllable for many, many years.
So just from a very high perspective, if we’re going to try to cure prostate cancer, the two mainstays of treatment at this point would be surgery to remove the prostate. Typically, these days that’s done robotically, which is a version of laparoscopic surgery, kind of a minimally invasive approach, or radiation treatments. And I always have to make sure that my patients understand, a lot of people confuse radiation with chemotherapy, and so I always have to say, “Chemotherapy is the medicine of the veins, makes you kind of feel sick, your hair can fall out. Radiation is going to be focused energy at prostate cancer.” They use it for breast cancer, brain cancers, things like that. But those are the two ways, surgery to remove the prostate, or radiation to essentially zap the prostate, as I put it, to try to cure prostate cancer.
Carol Gifford:
So is the protocol for men as part of their ongoing health is to get a PSA test whether they think they have prostate cancer or not? What’s the protocol, and at what age should they start doing that?
Dr. Steven Thoma:
So that was a little controversial a few years ago. Previously we would start screening men somewhere around 40, and we would just do it until the end of their days. And that was excessive, and we were finding that we were creating anxiety from false readings, and draining medical resources on men that didn’t need to be screened. So then there was a task force that unfortunately went a little too overboard, and said, “No one should ever be screened for prostate cancer.” And that obviously created problems in and of itself, because as we mentioned before, extremely treatable. So now there’s felt to be a really good happy medium. Typically, we start screening around 55. If you have a family history of it, you should probably start a little bit earlier, maybe around 50.
And they tend to say at around 70 you should consider discontinuing screening for prostate cancer, but that needs to be kind of a shared decision between the patient and their provider, whether it’s a primary doctor or a urologist. Because if you have a guy that is 75, but he’s in fantastic shape, he’s got a good chance at another 10 to 15 years of life, and those are going to be high quality years, you want to know if that guy has prostate cancer so that you can get ahead of that. On the flip side of that, if you’ve got a guy who’s 60, who’s in very bad shape, we don’t tend to worry about prostate cancer. Just because as most folks know, prostate cancer tends to move pretty slowly. So if you’re not thinking that that gentleman has too many more years ahead of them, you can kind of cross prostate cancer off as being a concern.
Carol Gifford:
So let’s talk about enlarged prostate. It was in the news recently that King Charles had an enlarged prostate, I don’t think we heard much more. But I know that’s something that you treat, right?
Dr. Steven Thoma:
Yes.
Carol Gifford:
And so what is it? What are the concerns with enlarged prostate? And what are the symptoms for a male? And then, again, what are some of the treatment options?
Dr. Steven Thoma:
Sure. So most men know that they have a prostate, they hear, “My dad had trouble with urination, he would always curse his prostate, et cetera, et cetera.” But not a lot know kind of the anatomy of it. And so the prostate sits right under the bladder, and I like to think of it almost like a donut. There’s a channel right down the middle of that prostate, the prostatic urethra. And so the urine has to go from the bladder through the prostate to get to the outside world. And as we get older, the prostate naturally enlarges, and so it can eventually cause obstruction. So as that channel gets narrower and narrower, kind of like a kinked hose or a clogged pipe, it can cause difficulties. Those typical symptoms are things like slow urine stream, having to wait to get started, feeling like you don’t empty well, getting up several times at night. But then it can also cause irritative symptoms as we call them. Things like going to the bathroom frequently, going urgently, maybe even not being able to make it in time.
And so those are the classic symptoms of enlarged prostate. And as far as treating enlarged prostate, unfortunately a lot of men out there, based off of studies, don’t really seek any sort of care at all. They just think it’s part of aging, and they just think it’s something they’re just going to have to deal with, and it can cause significant quality of life implications. And so as far as treating it, oftentimes we start with medications. There are several classes out there that can be very helpful for these symptoms. But for some guys, they don’t help as much as they’d like, or they might have side effects like many medicines do, or they just don’t want to be on a medicine. A lot of people just don’t want to do that. And so then there are several procedures out there that can help, it just depends on the preferences of that person and what their urologist feels is best for them.
Carol Gifford:
And so did you want to talk about that one particular procedure that you do called UroLift?
Dr. Steven Thoma:
Sure, yeah. So that is one of several that are out there, that’s one of my favorites. It’s always nice to have different tools in the toolbox. And so in the appropriately selected patients, a procedure like a UroLift can be very helpful. As part of evaluating who is a good candidate for what, patients often receive things like cystoscopy, so scopes into the bladder to take a look at the prostate from the inside, and sometimes we’ll even use ultrasounds to measure the size of the prostate. And that helps us to figure out what procedure or intervention might be the best for a particular patient. So as far as UroLift, about 90% of guys will find that they are a candidate for a UroLift. And it’s a procedure that’s thankfully very quick, takes maybe 15 minutes or so.
It can be done under some light sedation, so that you don’t have to be under a general anesthetic, it can even be done in an office setting at times. And so there’s often quicker recovery than some of the others, you go home the same day, very little chance of needing a catheter afterwards, usually somewhere around 10 to 15% chance of that. A lot of guys like that because with pretty much every other procedure for a prostate, it’s about a 100% chance. And then just a few days of laying low, taking it easy. But it can be very, very effective, and it can help men to improve their symptoms and get off of their medications in the vast majority of the time. So yes, it is one that we offer here at the Mason City Clinic, it’s one that I have done, I think over 300 at this point. So yeah, it’s been great. I mean, it’s been very effective.
Carol Gifford:
Now what are you doing? Are you pulling the prostate that is enlarged, you’re pulling it back, right?
Dr. Steven Thoma:
Sure. So when you think about the prostatic urethra, this channel that’s becoming clogged or blocked, we have the walls one side and the other, and they have essentially moved towards the midline. A lot of times we see kissing walls, or kissing lobes, or they’re touching each other. And so as you can imagine, when you try to pass urine through there, that’s difficult because there’s blockage. So the UroLift is a very small implant, almost looks like an H. So you have two metal tabs, and then perpendicular to those in between is a heavy duty monofilament suture. I like to think of it kind of like a heavy duty fishing line.
And the device that we use to deploy the UroLift implant, it’s all through scopes, so there’s no cutting on the outside. And what it does is it deploys it into the wall of the prostate on one side, and it compresses that wall. So it almost acts like a staple, an anchor, a dry wall anchor, some guys think about. But it grabs that wall and it compresses it down. So you do it on one side, and then you try to be as symmetrical as possible, you go to the opposite side, you do the same thing. And it pulls those two walls away from the midline, and then you just keep putting in pairs of implants until the entire prosthetic urethra has been pulled away from the midline to unobstruct that prostate.
Carol Gifford:
And how has that… I mean, what’s the success rate? I mean, you must talk and see patients after they’ve had this procedure, how’s it working for them?
Dr. Steven Thoma:
Sure, so I’ve had very good results. You ask success rates, and that’s difficult because everybody kind of gauges success differently. I would say very, very high. I mean, I would’ve phased it out a long time ago if I didn’t think that we were getting good results. And so some of the guys wonder, well, how long does it last? The data on that is still coming in, we know five years. The retreatment rate, meaning needing to go on medicines or have another procedure, somewhere in the 13 to 14% range. Which when you compare it to the gold standard, a surgery called a TURP, that’s somewhere around 11 to 12%. So pretty comparable.
And so success rate has been very high, durability has been very high. And one of the things that we haven’t touched on is why some of these other procedures, besides the gold standard TURP, why they even exist. TURPs can at times have impacts on things that are very important to men, most notably sexual function. And so UroLift has no impact on that. It doesn’t cause any sort of ejaculatory issues or erectile function issues, whereas a TURP can impact those things at times. And so when you have a patient that those things are important to him, and he otherwise is a good candidate for something that is not as invasive as a TURP, then things like UroLift are very attractive to that patient.
Carol Gifford:
That’s a very important distinction. So let’s talk a little bit about birth control, oftentimes women think they’re responsible for it, but there are options where men can participate. And one of those procedures is vasectomy. So talk to me a little bit about how you counsel men and their partners for vasectomy, if it’s appropriate. And again, what are the success rates for using that as birth control?
Dr. Steven Thoma:
Sure. So that is going to be the gold standard of birth control in men. It’s a permanent sterilization option, most men know that it can be reversed, but anytime I meet with these men, I always have to say, “You need to be pretty certain that this is what you want and your family is complete, you don’t want any further fertility. Because while it can be reversed, it’s not always successful.” But compared to permanent sterilization, kind of surgical procedures in women, it’s much easier for us men to do it. And so we definitely encourage men when their families are complete to consider this. When these patients come in, I tend to tell them, “The procedure for me, usually about 30 minutes, maybe 45 from the time I walk in to the time I walk out of there.” I tend to do these through a very small incision, maybe half inch or so, very small.
You can do it with just topical anesthesia, numbing guys up with things like lidocaine. We offer nitrous oxide, laughing gas helps quite a bit, but very minor procedure. And so we always tell guys to just take it easy for about three to four days afterwards. But beyond that, it’s very minor and extremely successful. You asked about success rates, different numbers are thrown out, but I tend to quote that the failure rate one in a thousand. Thankfully, I’ve never seen that one. I always knock on some wood on that one. But extremely successful, very minor procedure. And like I said before, it’s way less invasive than anything that a woman might have to try to have. So always nice to do that for your partner if that’s an option.
Carol Gifford:
So let’s talk about incontinence, I know that’s a big issue, and it affects men and women. So I know you treat that, and so I don’t know if you can do a quick overview of different types of incontinence, and then what some of the treatment options are for both men and women.
Dr. Steven Thoma:
Sure. So the two main umbrellas that are most often treated are going to be incontinence types called urge incontinence or stress incontinence. And people hear stress, I always have to say, “It’s not stress like anxiety. Stress as in that’s the type where if you cough, if you laugh, you sneeze, you get pressure in your abdomen, which then stresses the bladder and they end up leaking like that.” That’s a very common type in women, it’s a very rare type in men, unless they’ve had certain surgeries and things like that. But urge incontinence can be found in both men and women. Those are treated very differently because the root causes are very different, thankfully we can help with both of those types. With urge, that’s typically treated with medications. There are a couple of classes of medicines at this point that help with those, and they can be very successfully treated that way.
Unfortunately, not everybody responds well to medication, so then there are some other procedural based things that thankfully are very minor, but also very successful. People have heard of Botox injections, everyone’s heard of those for wrinkles, we actually use it in the bladder for those issues where urgency is severe and the medicines aren’t helping. For the stress incontinence, as I mentioned before, that is an anatomic issue. And so there are not any medicines for that, there are sometimes exercises that we offer, teach, physical therapy, biofeedback type things. But at times that requires surgical procedures. Some patients have heard of things like mid-urethral slings, or different sorts of anti-incontinence procedures that are out there. But yes, those are things that we can treat very successfully, and we encourage both patients and primary docs to be aware of those things, because a lot of people just think that’s something they just have to deal with. And it’s not, it is absolutely something that we can help with, so absolutely.
Carol Gifford:
So we talked about this earlier before we started the podcast, but I know that physicians, including yourself, do go out to clinics outside of Mason City. So I think you serve… What, a eighty-mile radius of Mason City?
Dr. Steven Thoma:
Oh, gosh, it’s probably more than that at this point.
Carol Gifford:
More than that?
Dr. Steven Thoma:
Yeah.
Carol Gifford:
Okay. So you participate, you go out to… Why do you think that’s important for patients in North Iowa that you go closer to their home? Even if they need surgery, they might have to come to the Mason City Clinic for that. Why is that important, do you think?
Dr. Steven Thoma:
Well, it’s for many reasons, but just being able to provide what we feel is high quality medical care to patients all over the state is going to be very important. Some of our patients are older or have extenuating circumstances where it’s very difficult for them to travel, and it’s great for us to be able to come to them so that their access to healthcare isn’t compromised, isn’t cut off from them. And it’s great also for us, from our clinic perspective, to be able to go and visit these outlying medical areas where most small towns have docs there, it’s nice for them to know that they have the support of our clinic as well. Because with these primary care providers, a lot of times they sometimes feel overwhelmed by some of the things that come in because they’re not a urologist, they’re not a ear, nose, and throat physician, and so…
Carol Gifford:
Or cardiologist.
Dr. Steven Thoma:
Yeah, exactly. And so they are very thankful that we are able to come and be a resource for them, they can come and ask us for help, and questions, and things. So for those reasons, it’s great that we’re able to go and visit patients closer to them rather than them having to come to us.
Carol Gifford:
And which areas do you visit on a weekly or bi-weekly basis?
Dr. Steven Thoma:
Sure. So the places that I personally go, I go as far west as Emmitsburg, I go to Algona, I go to Iowa Falls, was just there this morning, and I also go to Belmond, Iowa. But my partners go to other places that I don’t, Osage, Cresco, Hampton, Waverly, Charles City, there’s lots of places. You just draw a big circle around Mason City, and we’re hitting pretty much any significant town there. So yes, we have a very big footprint, which we like, we are happy to be able to help the patients of North Iowa and Southern Minnesota.
Carol Gifford:
So what do you think is the most important part of taking care of your patients?
Dr. Steven Thoma:
The most important part, I would say that would be them feeling comfortable with the care that they receive. I often get told, “Thank you for explaining these things.” A lot of times patients don’t fully understand what’s happening or why. And I think it helps to relieve that anxiety that comes with medical issues when you understand your problem. It’s not so much just to get a medicine and be told, “This will make it better.” When you know why things are happening to you, and what strategies we have to try to make them better. And one of the big things I like is giving options and helping educate those patients on how they can make the best decision for themselves. So that’s what I find most gratifying on a day-to-day basis, is not only helping those patients, but helping them feel comfortable with their decisions, and feel as though they made their decision.
Carol Gifford:
Got it, information is knowledge.
Dr. Steven Thoma:
Yeah, of course.
Carol Gifford:
Okay. Well, thank you Dr. Thoma for being on the program.
Dr. Steven Thoma:
Yeah, my pleasure, thank you for having me.
Carol Gifford:
Thank you for listening to Mason City Docs on Call. For more episodes, go to Mcclinic.com\radio-podcast.

 Ten years ago, my Mason City Clinic heart surgeon removed my expiration date
Ten years ago, my Mason City Clinic heart surgeon removed my expiration date Dean Haugen
Cardiology Patient
I used to visit the ER often with undiagnosed heart problems. During my last visit in 2004, they told me I probably wouldn’t make it another year. That’s when my doctor at Mason City Clinic found my mitral valve malfunction and surgically repaired it. I recently had my annual EKG exam and my cardiologist found no heart problems whatsoever. Which means I can keep raising my squash, musk melon and tomatoes.
Read More He’s the best doctor I’ve ever had – and I’ve had a lot
He’s the best doctor I’ve ever had – and I’ve had a lot Jansen Wyatt
Cardiology Patient
With no warning signs, Jansen Wyatt, 54, suddenly collapsed in his home last November. His daughter-in-law rushed him to the ER at Palo Alto County Health System in Emmetsburg, where they diagnosed a severe heart attack. Jansen was helicoptered to Mason City’s Mercy Medical Center. Samuel Congello, DO, a board-certified cardiologist with Mercy’s Heart and Vascular Institute.
Read More How do you handle kids if you can’t use your hands?
How do you handle kids if you can’t use your hands? Sandy Wagner
Plastic Surgery Patient
After years as a special education teacher handling children with significant disabilities and behavioral challenges, I began having limited use of my hands due to severe arthritis pain. I found myself fighting back tears every day because the pain was so bad. I could no longer enjoy one of my favorite hobbies, quilting, either. I met with Dr. René Recinos, a plastic surgeon from Mason City Clinic and recommended a procedure called arthrodesis.
Read More By replacing her arthritic hip and knee, Charlene can walk in the woods again without pain
By replacing her arthritic hip and knee, Charlene can walk in the woods again without pain Charlene Hanson
Orthopedics Patient
Retired school teacher Charlene Hanson used to love walking in the woods – until the pain and inflammation of arthritis took it away from her. Since she had heard such great things at church and in the community about Mason City Clinic’s Orthopedic Department and Dr. Darron Jones, she made them her choice to replace her arthritic hip and knee.
Read More Getting The Hip Replacement Surgery Done At 60 Was The Best Decision I Made
Getting The Hip Replacement Surgery Done At 60 Was The Best Decision I Made Roger Kuck
Orthopedics Patient
Roger was always very active, but a few years ago his hip started to bother him. When he would go to bed at night the pain was very severe. “I would have to lay on the floor and put my legs up on the couch to relieve the pain,” said Roger.
His orthopedic surgeon at the Mason City Clinic Dr. Darron Jones said, “I can give you cortisone shots, but this is a quality of life question.
 I trusted him 100 percent
I trusted him 100 percent Donna Drake
Plastic Surgery Patient
Donna Drake lived with a growing basal cell skin cancer (the most common skin cancer) on her lower eyelid for three years. A family practitioner at Franklin General Hospital recommended Mason City Clinic’s plastic and reconstructive surgeon, Dr. Mark Mulkey, who identified the cancer and performed the extremely delicate eyelid surgery to remove it and reconstruct her eyelid.
Read More Bunion pain stopped Melody in her tracks
Bunion pain stopped Melody in her tracks Melody Wagner
Podiatry Patient
Melody Wagner loved walking until severe pain from bunions stopped her cold. She found a board-certified podiatrist at Mason City Clinic’s Podiatry Department. Podiatrists perform leading-edge surgery for bunions and hammertoes, as well as advanced treatments for diabetic feet, heel pain, ingrown toenails and more. Melody was afraid of a painful procedure and a long recovery.
Read More I didn’t know the pain in my leg came from a ruptured blood vessel in my chest
I didn’t know the pain in my leg came from a ruptured blood vessel in my chest Lyle Miller
Cardiology Patient
One snowy night about seven years ago, I felt a sudden pain in the back of my leg. I thought I could shake it off and went out to shovel some snow. After a few minutes, I went back inside and collapsed. My wife called 911 but the ambulance couldn’t get to me because of the snow. My neighbors used snow blowers to clear the road and my driveway so the ambulance could get to me.
Read More No more sour grapes about knee pain for me
No more sour grapes about knee pain for me Gordon Lubbers
Orthopedics Patient
I injured my knee as a teenager and had surgery. Then, as I got older, the pain returned and began affecting my routine and overall enjoyment of life. My doctor referred me to Darron Jones, MD, an orthopedic surgeon. After a thorough exam, he said I was a candidate for knee replacement. I had the procedure in late January 2014 and was back among the grapes by the beginning of March.
Read More I Wanted To Dance Up A Storm At My Two Daughters Weddings, And I Did!
I Wanted To Dance Up A Storm At My Two Daughters Weddings, And I Did! Sheryl Borcherding
Orthopedics Patient
We have a lot of flower gardens on our acreage, and I was having problems kneeling to weed. I couldn’t walk long distances anymore and it was painful to get in and out of the car, walk up and down the stairs. Simple everyday tasks were hard. Eventually I was limping and in a great deal of pain.” said Sheryl Borcherding of Emmons, MN.
Read More I Now Can Play Football And Basketball With My Grand Nephew.
I Now Can Play Football And Basketball With My Grand Nephew. Jane Papouchis
Orthopedics Patient
Jane, 70, a retired nurse, is a very active person. She is a mother of one daughter and son in law, and has lots of 4 legged kids: guinea pigs, goats, Newfoundland dogs and 10 cats. I suffered with knee pain for a long time and would always take extra strength Ty-lenol.
Read More I Was Given 23 Years Of My Life…And Counting
I Was Given 23 Years Of My Life…And Counting Gene Wagler
Cardiology Patient
Gene Wagler, a special needs teacher from Clear Lake, didn’t have a history of heart problems before his heart attack 23 years ago. Gene said, “I didn’t feel any pain that day but I had a “gnawing” sensation in my chest. Within hours Gene was in the Mercy One-North Iowa ER and Dr. Sam Congello, an interventional cardiologist.
Read More I feel great and have none of the heartburn I had for so many years and have lost 12 pounds.
I feel great and have none of the heartburn I had for so many years and have lost 12 pounds. Kathleen Hanna
GERD Surgical Patient
Kathleen Hanna, 60, is a mother of four, grandmother of nine and a para-assistant at Forest City Elementary School. “I had heartburn with regurgitation for 40 years, have had an ulcer, and have been on heartburn medication for about that long too.” Having been on heartburn medication for many years her physician was becoming worried that it was affecting the function of her kidneys.
Read More I feel great. The surgery was easy. Now I can fully enjoy my life with my wife – we garden, bike and visit with our three grown children and three grand-daughters.
I feel great. The surgery was easy. Now I can fully enjoy my life with my wife – we garden, bike and visit with our three grown children and three grand-daughters. Duane Obanion
GERD Surgical Patient
In March 2019, Duane Obanion, 68, a farmer outside of Mason City, Iowa had an acid reflux attack. He aspirated into his lungs and got pneumonia. “I was in New York visiting my daughter when it happened and I ended up in the Urgent Care Center. When I got home I went to my family doctor and she put me in touch with Dr. Matthew Fabian, a general surgeon at the Mason City Clinic”.
Read More After Breaking Her Wrist In A Fall, Hampton Woman Gets Full Mobility of Her Hand And Wrist Back!
After Breaking Her Wrist In A Fall, Hampton Woman Gets Full Mobility of Her Hand And Wrist Back! LeAnn Strother
Plastics & Reconstructive Surgery Patient
In February 2019, LeAnn Strother 65, who is left-handed, fell and broke her left wrist. Because it was a complicated break she was referred into Dr. Rene Recinos, a plastics and reconstructive surgeon, and hand specialist at the Mason City Clinic for surgery. Most concerning for LeAnn was if this injury would impact all of the things she loves to do with her hands in the future?
Read More Dr. Scherb and his team are amazing
Dr. Scherb and his team are amazing Dan Rodemeyer
Orthopedic Patient
Dan Rodemeyer of Hampton, was at work when the unexpected happened. While on the loading dock, a 4,000 pound steel I-beam fell onto his foot. Dan said, “I was wearing steel toe boots, but the sheer weight of the steel beam crushed my foot and broke two of my toes. It was extremely painful to say the least.”
Dan initially went to the emergency room in Hampton. His foot had very severe soft tissue compression injuries, and there was an internal wound that was causing extreme swelling and pain. Although his big and second toe were broken, thankfully they were not compound fractures.
 Dr. Mulholland Has A Great Team And They Know Exactly What They Are Doing
Dr. Mulholland Has A Great Team And They Know Exactly What They Are Doing Paul Bruns
Urology (Prostate Cancer)
Paul Bruns of Clear Lake, a retired restaurateur and businessman, went to his Medicare screening with his family physician at the MercyOne Family Clinic in Clear Lake. To Paul’s surprise his physician called him back to let him know that his PSA count (protein in his prostate) was very high and that he needed to see a urologist as soon as possible.
Read More I would recommend Dr. Henrich to anyone.
I would recommend Dr. Henrich to anyone. Lisa Fuller
Podiatry (Dr. Henrich)
I am back to work on my feet everyday, and I walk my dog everyday. I don’t have any pain. Lisa Fuller, a mother of three from Algona, is on her feet a lot. “I own a can redemption center with my daughter and I am walking and moving eight hours a day. I used to come home with my feet swollen red and in pain. Now when I come home, I go take my dog for a long walk,” Lisa said.
Read More Iowa Falls Woman In Full Kidney Failure, Now Planning A Hiking & Fishing Trip Out West
Iowa Falls Woman In Full Kidney Failure, Now Planning A Hiking & Fishing Trip Out West Cindy Wingler
Cindy Wingler, 55, was returning from a trip out west with her boyfriend when she didn’t feel well and went to the ER at Hansen Family Hospital in Iowa Falls. She was nauseous and fatigued, and thought perhaps she was having another urinary tract infection which she had many of in her lifetime.
Read More Mason City Woman Back On Her Feet Again After Hammertoe Surgery
Mason City Woman Back On Her Feet Again After Hammertoe Surgery Rebecca (Becky) Groh
Rebecca (Becky) Groh, 64, only goes to one podiatrist in Mason City and that is Dr. Scott Donohoe.
“I have been to Dr. Donohoe three times - for my right and left foot bunions, and hammertoes, and recently he fixed a hammertoe on my left foot that was really bothering me.
 Charles City Woman Finds Relief From Sleep Apnea Symptoms and CPAP mask with New Procedure Called Inspire Therapy
Charles City Woman Finds Relief From Sleep Apnea Symptoms and CPAP mask with New Procedure Called Inspire Therapy Janet Stangl
Janet Stangl, 64, a retired administrative assistant from Charles City, was diagnosed with sleep apnea in 2006. Said Janet, "I was in the severe sleep apnea zone. I stopped breathing 30-50 times per hour during the night. I was prescribed the CPAP.
Read More Local man who struggled with the chronic symptoms of sleep apnea gets significant relief with new implantable device
Local man who struggled with the chronic symptoms of sleep apnea gets significant relief with new implantable device Keith Messenger
Keith Messenger, 44, a business owner in Mason City, was not getting quality sleep, and it was having an effect on his daytime productivity. “For five years or more I would crash (fall asleep) by 12 noon everyday.” Keith was diagnosed with sleep apnea; he was told that his tongue would fall back while he was sleeping blocking his airway during the night. He was prescribed the CPAP machine. Said Keith, “I tried 16 or 17 CPAP face and nose masks. The CPAP was so loud and the masks wouldn’t stay on my face. I was also prescribed a mouthpiece and that didn’t work either.”
Read More Garner woman says her ‘Tummy Tuck’ not only gives her self confidence, it’s the motivator for staying healthy.
Garner woman says her ‘Tummy Tuck’ not only gives her self confidence, it’s the motivator for staying healthy. Renee Denny
Renee Denny, 59, of Garner, Iowa, a retired school administrator, wants to be a healthy and active grandmother one day.
“Five years ago I had gastric bypass surgery and lost 90 lbs. I started at 240 lbs. Although I was pleased with the gastric bypass results, some of my skin was loose and sagging, and was getting caught up in my belly button and creating infections,” said Renee.
 Local Woman Gets A Total Knee Replacement Enabling Her To Step Back Into The Joys Of Her Life!
Local Woman Gets A Total Knee Replacement Enabling Her To Step Back Into The Joys Of Her Life! Suzanne Johnson
Suzanne Johnson, 74, of Mason City, had been struggling over the last few years to do the things she loves to do.
“I couldn’t do any type of walking. If my husband and I were going to a fair or flea market, I would always have him bring the electric scooter for me. It was limiting — not the day to day things around the house — but going out and doing the things that I love to do,” said Suzanne.
 Garner woman gets back to active life quicker after having a new & innovative bunion surgery, performed only at the Mason City Clinic.
Garner woman gets back to active life quicker after having a new & innovative bunion surgery, performed only at the Mason City Clinic. Jane Peterson
Jane Peterson 68, of Garner Iowa loves to golf, but it was getting harder and harder to do it with the bunions she had on each foot. “My feet would just get tired much sooner when I was golfing. And I was working full time at a factory, standing all day on a cement floor which became very painful. I just wanted to get my feet into shape by retirement so I could continue to play golf comfortably and be active with my 10 grandkids,” said Jane.
Read More Weight Loss Surgery Helped A Fort Dodge Man Lose 100 Pounds, Bring His High Blood Pressure To Normal, and Eliminate Knee Pain
Weight Loss Surgery Helped A Fort Dodge Man Lose 100 Pounds, Bring His High Blood Pressure To Normal, and Eliminate Knee Pain Scott Kuhlman
In 2020, Scott, 54, of Fort Dodge, at 5’8” weighed 342 lbs., his blood pressure was so high his doctor told him he was at high risk for a stroke, and he had extreme knee pain. Today Scott weighs 213 lbs., his blood pressure is normal, and all of his knee pain is gone.
Read More Mother Of Four And Special Education Teacher Loses 100 Pounds Through Gastric Bypass Surgery, And Feels Happier Than Ever
Mother Of Four And Special Education Teacher Loses 100 Pounds Through Gastric Bypass Surgery, And Feels Happier Than Ever Lisa Buss
Clear Lake resident and special education school teacher Lisa Buss, 56, reached a high of 280 pounds. Said Lisa, “When I was younger I was able to eat anything and not gain weight. Then as I got older and had my kids I started getting heavier and heavier, and it was very hard for me to lose the weight on my own.” On a 5’7” height Lisa was 150 pounds over a healthy weight.
Read More New Aortic Valve Replacement Procedure Called TAVR Giving Patients Their Quality of Life Back
New Aortic Valve Replacement Procedure Called TAVR Giving Patients Their Quality of Life Back Rosalyn Barron
Rosalyn, 83, of Mason City, is a mother of three, grandmother of six, and was a regis-tered nurse at Mercy for 30 years.
“Over the last three years I was short of breath and getting bad chest pains. I had a stent placed in September 2021 for some blockage in one of my arteries, but I was still getting these worrisome symptoms,” said Rosalyn.
 Clear Lake Man Treated Successfully For Atrial Fibrillation Credits Cardiologist Dr. Michael Spooner For Managing His Care So Well
Clear Lake Man Treated Successfully For Atrial Fibrillation Credits Cardiologist Dr. Michael Spooner For Managing His Care So Well Vern Toohey
In late 2019 Vern Toohey, 59, of Clear Lake, was having very rapid heartbeats and feeling exhausted. Said Vern, “I couldn’t walk across the house without feeling really tired.”
Read More Self-Detection Helped Mason City Woman Catch Her Breast Cancer Early Said Mason City Clinic Surgeon Caitlin Lund, DO, Was Compassionate & Kind
Self-Detection Helped Mason City Woman Catch Her Breast Cancer Early Said Mason City Clinic Surgeon Caitlin Lund, DO, Was Compassionate & Kind Gina Chenowith
In April 2022, mother of two, grandmother of five and retired business teacher, Gina Chenoweth, 67, of Mason City, noticed a lump in her breast. “I was pre-occupied with planning a trip to Ireland and I had had a fibroid cyst for a long time so I really wasn’t concerned. But then I showed it to my sister Kim who told me I should not wait and get it looked at right away,” said Gina.
Read More Harold Lewis – Jennifer McCambridge, PA; Samuel Congello, DO – Cardiology (Stents, Defibrillator)
Harold Lewis – Jennifer McCambridge, PA; Samuel Congello, DO – Cardiology (Stents, Defibrillator) Harold Lewis
Harold Lewis, 69, retired three years from the Winnebago company, a father of five and a grandfather of nine, remembers how he felt five years ago. “I was waking up at night and couldn’t breathe. I was also very tired and fatigued during the day. I went to see my family physician at MercyOne North Iowa Dr. (Phruns)? and then Dr. Brett Mulkey. They recommended that I go see Jennifer McCambridge, PA, in the cardiology department at the Mason City Clinic.” said Harold.
Read More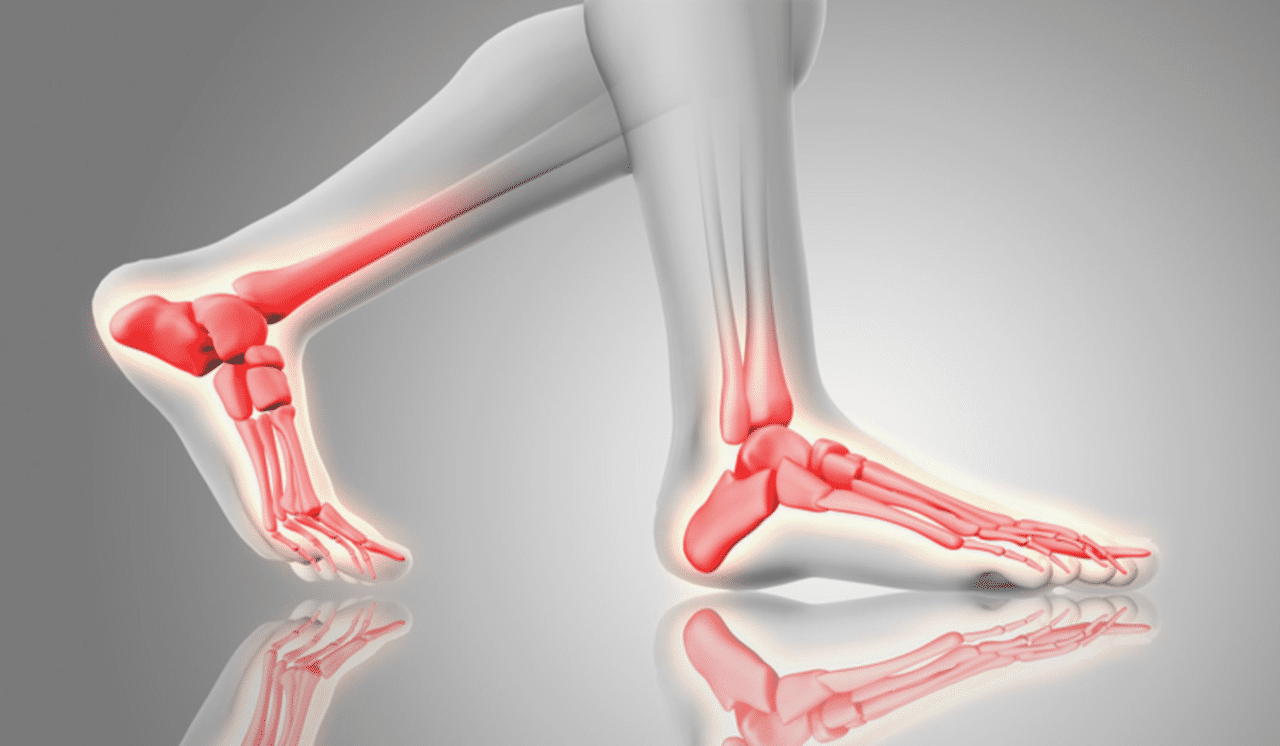 Emmetsburg Man Had Ankle Replacement & Has Increased Mobility, Less Pain Credits Orthopedic Surgeon & Podiatrist At MercyOne North Iowa Specialty Care at Mason City Clinic For His Successful Surgeries
Emmetsburg Man Had Ankle Replacement & Has Increased Mobility, Less Pain Credits Orthopedic Surgeon & Podiatrist At MercyOne North Iowa Specialty Care at Mason City Clinic For His Successful Surgeries Larry
It was 50 years ago when Larry, 71 years old, from Emmetsburg, Iowa, was in a motorcycle accident. His ankle was crushed and his knee broken under the knee cap.
Read More Three surgeries in a year has this Woden farmer back to his daily work and golf game. Credits orthopedic surgeon Dr. Michael Crane for helping him feel ‘fantastic’
Three surgeries in a year has this Woden farmer back to his daily work and golf game. Credits orthopedic surgeon Dr. Michael Crane for helping him feel ‘fantastic’ Mike Missman
Mike Missman, 63, is a corn and soybean farmer in Woden, Iowa. It’s a physical job. “My left knee was giving me problems for many years. I felt unsteady on slippery ground in winter weather, and was in alot of
discomfort doing ‘grain climbs’ (walking up and down the stairs of the grain elevators). I was also favoring my right knee which started to bother me as well. In addition to my knees, my pinky and ring finger on my left hand and pinky and index finger on my right hand curled touching my palm. After awhile there were things that I couldn’t do with my hands
including certain mechanical functioning with tools. My grip was not tight, which also affected my golf game,” said Mike.
 Clear Lake Woman Finds Joy In Outdoor Activities Again. Pain Specialist at the Mason City Clinic Helped Relieve Her Hip Arthritis Pain, Without Surgery.
Clear Lake Woman Finds Joy In Outdoor Activities Again. Pain Specialist at the Mason City Clinic Helped Relieve Her Hip Arthritis Pain, Without Surgery. Deborah Wessels
Clear Lake resident Deborah Wessels, 69, is a proud Iowa State Cyclone alum, mother of two and grandmother of three, and enjoys being active. Deborah loves to hike, bike, golf and travel.
“For the last two years I have had a sharp pain in my left buttock. It was localized, but it started to really interfere with my activities. I used to walk three miles a day and I couldn’t do that anymore without extreme pain. I went to New York City with a college friend and we had to stop so much while walking around the city it just didn’t feel normal,” said Deborah.
 Fredericksburg Woman Gets High Quality Care Close To Home
Fredericksburg Woman Gets High Quality Care Close To Home Elaine Westin
Mother of two and grandmother of four, Elaine Westin, 68, of Fredericksburg was struggling to do many of the activities she loves.
Said Elaine, “My husband and I went on a cruise up the east coast into Canada to see the Fall foliage and I couldn’t do many of the walking tours. My knee was weak and the pain went into my back. My flower beds suffered last summer because it was hard for me to bend over and weed. I couldn’t pick my strawberries. I even had trouble working the pedal on my sewing machine. Climbing the bleachers in the arena to watch my grandson play sports was painful and difficult. And I was not steady on my feet holding my 5 month year old grandson and I want to feel steady and sure of myself.”
 Partial Knee Replacement Allows Iowa Woman To Live Without Pain
Partial Knee Replacement Allows Iowa Woman To Live Without Pain Deann Meirick
Deann Meirick, 54, of Elma, Iowa, is a housekeeper and laundry aid at a nursing home facility. She is on her feet a lot. Said Deann, “Both of my knees had been bothering me. I knew it was arthritis, but all of a sudden, my left knee was hurting to the point that I couldn’t put any weight on it.”
Read More Klemme resident on road to recovery after ankle surgery
Klemme resident on road to recovery after ankle surgery Chad
Chad Boyington, 52, a forklift operator from Klemme, Iowa, and his wife Darci of 23 years, love to travel. One of their favorite spots is near Hatfield, WI. where they rent a cabin three times a year, bring up their UTV and enjoy the great outdoors.
Read More
 George Mathews
George Mathews 



